Tuberculosis
Tuberculosis is an infectious disease usually affecting the lungs.
Tuberculosis in Sri Lanka
District wise annual TB cases – 2012 to 2019

Summary
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis which primarily affects the lungs. Currently TB is endemic in Sri Lanka with a comparatively low burden of cases. It is observed that TB increases with the increase in temperature and wind speed. National Programme for Tuberculosis Control & Chest Diseases (NPTCCD) is the central organization for control and management of TB in Sri Lanka.
Introduction
Tuberculosis (TB) is an airborne, chronic infectious disease caused by Mycobacterium tuberculosis. The spread of TB occurs when infectious particles expelled from a source case is inhaled by an individual. TB usually affects the lungs but it can affect other parts of the body, such as brain, kidneys or the spine. Despite being a vaccine preventable disease a significant number of TB cases are reported in Sri Lanka and globally.
Classification of Tuberculosis based on the Anatomical Site of the Body
- Pulmonary tuberculosis (PTB)
Any bacteriologically confirmed or clinically diagnosed case of TB involving the lung parenchyma or the tracheobronchial tree with or without the involvement of any other organs in the body.
- Extra pulmonary tuberculosis (EPTB)
Any bacteriologically confirmed or clinically diagnosed case of TB involving organs other than the lung parenchyma or tracheobronchial tree, e.g. pleura, lymph nodes, abdomen, genitourinary tract, skin, bones and joints, meninges.
Recent Status of Tuberculosis in Sri Lanka
Per WHO estimates (Global Report 2018) Sri Lanka, with a population of 21 million, is considered a relatively low burden TB country with an estimated TB incidence of all forms of TB of 64/100,000 population, an estimated MDR TB incidence of 0.42/100,000, an estimated incidence of HIV/TB of 0.23/100,000 and TB mortality, excluding TB-HIV, of 3.2/100,000 population. The actual reported TB incidence was 47/100,000 in 2017 leading to an overall gap in case notification of about 3000 to 4000. In 2018, Sri Lanka notified 8856 patients (up from 8511 the previous year) of all forms of TB of which 4181 (47%) were bacteriologically confirmed, 2431 (27%) were EPTB, and 591 (6.7%) were retreatment cases. The majority of cases occur in the Western province (40%), with most reported from Colombo (25%). It is also observed that children contribute to 3% of the notification rate.
Tuberculosis in Sri Lanka

Average TB Cases by Quarter for 2013-2017

The quarterly analysis carried out for the TB case data from 2013-2017 shows,
- 1st quarter – highest average cases are observed for Colombo, followed by Gampaha, Kandy, Ratnapura, Galle, Kurunegala
- 2nd quarter – highest average cases are observed for Colombo, followed by Gampaha, Kandy, Ratnapura, Kurunegala, Galle
- 3rd quarter – highest average cases are observed for Colombo, followed by Gampaha, Kurunegala, Galle, Kandy, Ratnapura
- 4th quarter – highest average cases are observed for Colombo, followed by Gampaha, Kandy, Kurunegala, Galle, Ratnapura
Colombo has its highest peak in the 4th quarter
- Overall – The highest average is for Colombo followed by Gampaha district throughout the four quarters while lowest shown in Kilinochchi, Mannar, Mullaitivu respectively.
- Third Quarter shows high averages compared to other quarters.
- Lowest averages are shown in the second quarter.
From 2013-2017, the total number of cases nationally ranges from 1599-2098. The highest number of cases is observed in the 4th quarter of 2017 and the lowest in the 2nd quarter of 2014 (Figure 3).

Impacts of Climate and Pollution on Tuberculosis
TB notifications have been observed to parallel the temperature amplitudes in some Asian countries.
Seasons may affect TB transmission and case notifications in a variety of ways. Temperature and precipitations determine the amount of time spent indoors, and thus the transmissibility of Mycobacterium tuberculosis. Seasons shape workload and health-seeking behavior, as precipitation may hinder access to healthcare facilities when TB causes ill-health, and season-dependent nutrition and metabolism may influence response to infection with M. tuberculosis.
In a study carried out in Beijing, China, it was found that the TB incidence was negatively correlated with the concentration of inhalable particulate matter, sulfur dioxide, or nitrogen dioxide. Precipitation, atmospheric pressure, and relative humidity had negative effects on TB incidence by indirectly lowering the concentrations of inhalable particulate matter and sulfur dioxide. By contrast, wind speed had a significant positive correlation with the incidence of TB. Temperature and wind speed had positive effects on TB incidence by improving the concentrations of inhalable particulate matter and sulfur dioxide.
Climate and air quality are potential regulators of the incidence of TB. The improved air quality contributes to the decline of incidence of TB in Beijing. The impact of climatic indicators on the incidence of TB is mainly regulated by the environment.
Management and Control of Tuberculosis
National Programme for Tuberculosis Control & Chest Diseases (NPTCCD) is the central organization of the Ministry of Health responsible for controlling and preventing tuberculosis (TB) and other respiratory diseases throughout Sri Lanka. it functions through a network of chest clinics, laboratories, chest wards and hospitals. The work of the NPTCCD is under the supervision and guidance of the Director General of Health Services (DGHS) and the Deputy Director General of Public Health Services (DDG-PHS). With a moderate burden of TB and rising number of cases of respiratory diseases, TB and respiratory diseases remain as a serious public health concern.
The NPTCCD, originally named Tuberculosis Commission was established in 1910 to practice methodical approaches in TB control activities. The NPTCCD aims at spreading awareness of chest diseases and their health impacts at various social levels.
National Policy of the NPTCCD
- Notification of all tuberculosis patients
- Provision of treatment, free of charge to all patients diagnosed with tuberculosis according to National Policy guidelines.
- Registration of all the tuberculosis patients in District Chest Clinics
- Provision of free sputum microscopy services to all tuberculosis patients
- Provision of DOTS throughout the whole period of treatment.
Objectives of the NPTCCD
- To ensure that every patient with tuberculosis or a respiratory disease has access to effective diagnosis, treatment, cure and rehabilitation.
- To interrupt the transmission of tuberculosis.
- To prevent the emergence of drug resistance.
- To reduce the social and economic toll caused by tuberculosis and other respiratory diseases.
NPTCCD Website: https://www.nptccd.health.gov.lk/
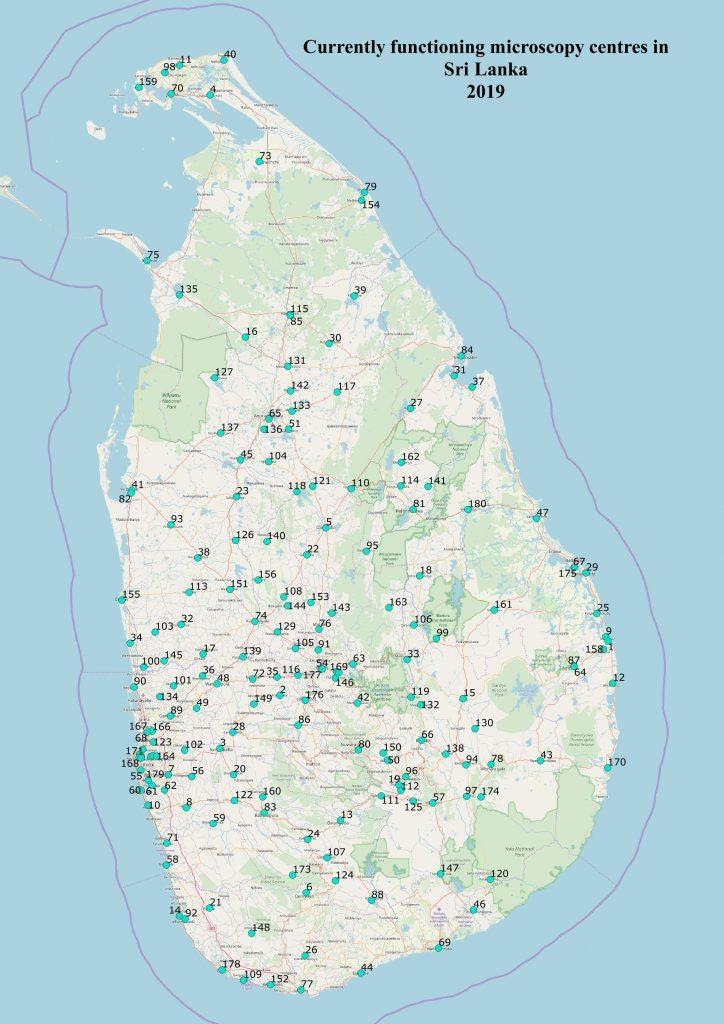
NPTCCD carries out its control activities through 26 district chest clinics and many microscopy centers located throughout the island. There are 26 districts with 13 TB wards and one tertiary care TB hospital with a specialized multi drug resistant TB (MDR TB) ward of 10 beds. The National TB Reference Lab is a BSL 3 lab with culture and DST capability; there are four Intermediate Reference Labs with culture capability and there are 31 Gx machines in the country.
References
National Programme for Tuberculosis Control and Chest Diseases, Ministry of Health, Nutrition & Indigenous Medicine Sri Lanka. (2018). Annual Report. http://www.nptccd.health.gov.lk/wp-content/uploads/2020/06/Annual-Report-2018-Mail.pdf
Zaman K. (2010). Tuberculosis: a global health problem. Journal of health, population, and nutrition, 28(2), 111–113. https://doi.org/10.3329/jhpn.v28i2.4879
N. Naranbat, P. Nymadawa, K. Schopfer, H. L. Rieder (2009). Seasonality of tuberculosis in an Eastern-Asian country with an extreme continental climate. European Respiratory Journal, 2009.
Zhang, C. Y., & Zhang, A. (2019). Climate and air pollution alter incidence of tuberculosis in Beijing, China. Annals of epidemiology, 37, 71-76.
Mase, S. (2019) RGLC Country Support Mission Report, WHO SEARO. https://www.who.int/docs/default-source/searo/tuberculosis/rglc-report-sri-lanka-2019-july.pdf?sfvrsn=6ef508f7_2
