MALARIA
OVERVIEW
ABOUT MALARIA
Malaria is a fatal infectious disease caused by parasites and is transmitted to people through the bites of infected female Anopheles mosquitoes. It is preventable and curable.
The symptoms of Malaria usually appear after 10-15 days of a mosquito bite. The mild symptoms are fever, headache and chills. In severe cases, it can cause seizure, coma or death.
People who are at risk to contract the virus are infants, children under 5 years of age, pregnant women, and patients with HIV/AIDS, non-immune migrants, mobile populations and travelers.
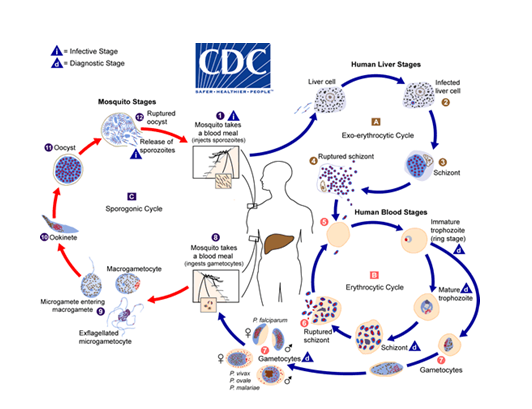
There are four types of human malaria: Plasmodium vivax, P. malariae, P. ovale and P. falciparum. P. vivax and P. falciparum are the most common forms. The Malaria parasite develops in the hosts both humans and in the female Anopheles mosquitoes.
The parasite changes through several life stages even while in the human host, at different stages of its life cycle. In addition, the parasite has developed a series of strategies that allow it to confuse, hide, and misdirect the human immune system.
MALARIA IN SRI LANKA
RECENT STATUS OF MALARIA IN SRILANKA
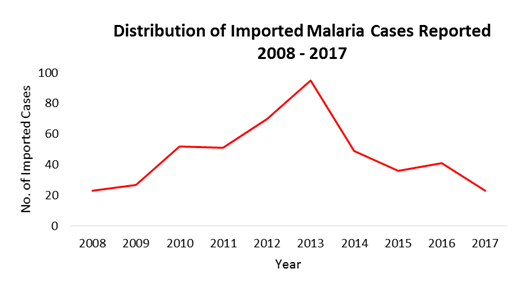
Globally 38 countries have been certified ‘Malaria-free’ including Sri Lanka. Sri Lanka being a tropical country has high receptivity and high vulnerability for vectors to breed. Though Sri Lanka eliminated malaria there have been imported cases resurging. The last reported indigenous case was reported in October 2012. There is a loss of awareness among the public, therefore surveillance of the vectors and prevention and re-introduction methods should be sustained.
History of Malaria in Sri Lanka
Malaria was prevalent in the 1900s in the country. There were many epidemic episodes in the past while the peak in the 1930s recorded about 5.5million cases and 80,000 deaths in Sri Lanka. (Malaria free Sri Lanka Report). After the introduction of DDT (Dichlorodiphenyltrichloroethane) in 1946, there was a gradual decline in the number of cases in the 1960s. Later DDT being resistance, the introduction of other substances like Malathion and artemisinin-based combination therapy (ACT), Malaria was brought under control with few cases and deaths being reported in the subsequent years.
Role of Climate, Hydrology and Environment
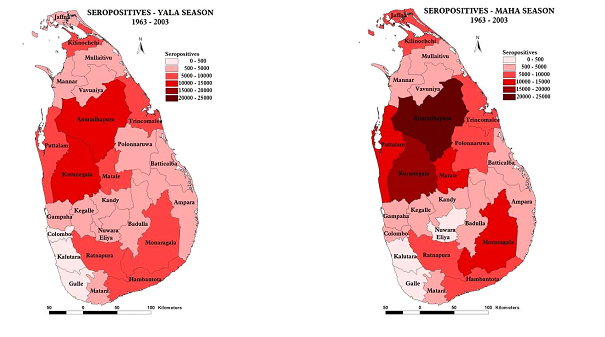
The climatic factors such as Rainfall, Streamflow, Temperature, Relative humidity influences Malaria. Sri Lanka being a tropical country is a favourable environment for vectors. Under dry climatic conditions, it is more prevalent. Therefore, Malaria was widely spread densely in the northern and southern part of the country over the years. There is a seasonal effect on Malaria as it surged in the Maha season.
Malaria elimination and Re-emergence
Sri Lanka is certified as a Malaria Free country in 2016 by WHO. Though Malaria was eliminated in Sri Lanka in 2018 a native was infected by malaria as a result of local transmission from an infected foreign migrant labourer.
There was no local transmission of Malaria in Sri Lanka for 6 consecutive years after elimination. Malaria cases are prevalent as imported cases are being reported. This is evidence that people have less know-how on malaria as it is not severe as compared to the past. Though Malaria is eradicated it is considered a re-emerging disease in Sri Lanka.
Control Programs
Here we focus on the time frame of Malaria and its effects and the steps and strategies taken to eradicate by health-care staff in remote areas, policies and investments in health care, the support of technology to achieve a Malaria free status in Sri Lanka. The establishment of the Anti-Malaria Campaign (AMC) and the role of international organizations, such as WHO to mitigate the disease is also presented.
Risk Management
Sri Lanka has a favourable breeding ground for vectors. Therefore, there is a higher chance of re-emergence. The methods used to prevent an outbreak and the strategies used to control and re-introduction of the disease at present is given below. We also briefly present the parasites responsible for causing malaria and the Life cycle of Malaria and the uniqueness of its cycle and the environment in which the malaria vectors breeds.
Vulnerability and Susceptibility
Environmental, socioeconomic, demographic, biological, cultural, and political factors contribute to malaria risk and vulnerability. Pregnant women and children under 5 particularly are recognized as vulnerable for Malaria. Vulnerability to malaria has a geographic aspect and adverse risk factors such as type of housing, economic activity, and age distribution. Climate influences the exposure and vulnerability and the susceptibility is enhanced due to malnutrition during droughts. Vulnerability assessment has to be conducted to delineate the geographic location of the epidemic-prone populations along with other demographic and socio-economic characteristics that lead to susceptibility.
Research on Malaria
Our past works on Analysis of impacts of climate and its variability on Malaria and its transmission, the Sri Lankan scenario are compiled under the regional spread and seasonality and the role of Malaria with climate, hydrology and environment and those vulnerable and the contributing factors are discussed.
GLOBAL OVERVIEW OF MALARIA
Global status of Malaria
Malaria is more prevalent in the African region and South-East Asia, Eastern Mediterranean, Western Pacific, and America are also at risk of contracting the disease. According to the WHO’s World Malaria Report 2019, there were no global gains in reducing new infections over the period 2014 to 2018. A child dies due to malaria every 2 minutes and each year 200 million cases are being reported and nearly as many people died from malaria in 2018 as the year before.
Impacts of Malaria
Though malaria is a deadly disease it can be prevented. Malaria has caused devastating famine within communities, killing thousands and undermining the development of the countries. The impacts of malaria can be from mild to severe. In the worst cases, it affects the fetus and causes seizures, coma, and death.
The Susceptibility
People who are at risk are the vulnerable communities who have bottlenecks due to health financing. The ones particularly susceptible are pregnant women and children under 5 years of age. Environment, Hydrology, and climate plays a role and those residing within this region are at risk to get malaria.
References
Baer K, Klotz C, Kappe SH, et al. 2007; (11):e171, Release of hepatic Plasmodium yoelii merozoites into the pulmonary microvasculature. PLoSPathogens,Life cycle of Malaria at https://www.malariavaccine.org/malaria-andvaccines/vaccinedevelopment/life-cycle-malaria-parasite. Accessed on August 3rd 2020 ……..
Center for Disease Control and prevention (CDC), 16 July 2020, Life cycle by GlobalHealth, Division of Parasitic Diseases and Malaria. Accessed on August
2,2020………https://www.cdc.gov/malaria/about/biology
WHO, 26 July 2022, Factsheet on Malaria https://www.who.int/news-room/fact-sheets/detail/malaria
World Malaria Report (2019). Global Malaria Programme World Health Organization.Geneva.
Karunasena, V.et.al 2019. The first introduced malaria case reported from Sri Lanka after elimination: implications for preventing the re-introduction of malaria in recently
eliminated countries. Malaria journal, 18(1), p.210.
